Over the past century, humanity has grown increasingly fascinated by the possible benefits of consuming all sorts of pills and potions to lose weight. The newest wave of this craze has come in the form of injectable medications like Ozempic and Wegovy.
The Food and Drug Administration approved Ozempic for Type 2 diabetes in 2017. Susan Yanovski, a physician and nutrition specialist at the National Institute of Diabetes and Digestive and Kidney Diseases, told ScienceNews that although “it’s still early days,” she has never seen such excitement surrounding a drug line. Considering that these drugs achieve results approaching weight-loss levels previously only possible through bariatric surgery, there’s even more reason to be interested. However, many questions remain about how exactly the drugs work, who should be taking them, how long they should be taken for, as well as what side effects users should be wary of.
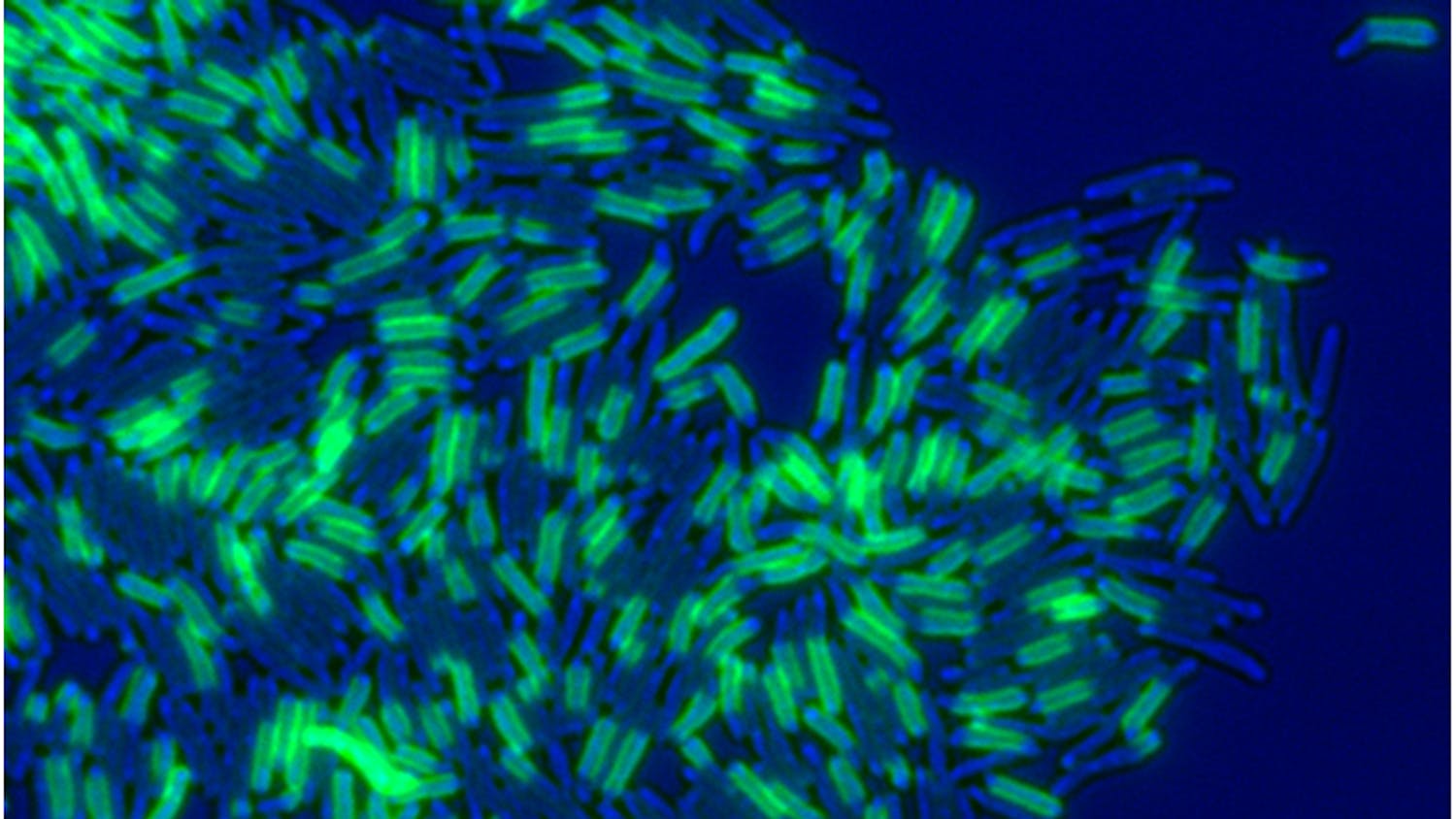
Ozempic and Wegovy are both brand names for the drug semaglutide. However, Wegovy has a higher maximum dose and has been specifically approved for weight loss, while Ozempic is intended for Type 2 diabetes. Semaglutide imitates GLP-1, the gut hormone that the body releases after the individual eats. GLP-1 stimulates the secretion of insulin, which facilitates the movement of glucose into the body’s cells to create energy. Thus, the drug causes the body to mimic a sense of satisfaction and satiation. In a double-blind trial, results were reported that after 16 months, people with diabetes taking a high weekly dose lost about 15% of their body weight.
In addition, semaglutide offers compelling possibilities for assuaging other health problems it was not initially intended to treat. Dr. A. Michael Lincoff, a cardiologist at Cleveland Clinic, conducted a 40-month drug trial with 17,000 participants. Weekly drug injections were shown to lower the risk of heart attacks, strokes and death due to cardiovascular disease by up to 20%. Health incidences caused by cardiovascular disease were noticeably reduced when participants took semaglutide compared to a placebo. This finding could be a groundbreaking advancement in treating the leading cause of death in the world.
A less intuitive benefit of semaglutide may be curbing addictive behaviors such as smoking, vaping and drinking. Dr. Lorenzo Leggio is studying the link between semaglutide and addiction, having published a study showing that semaglutide reduces alcohol drinking in rodents. Leggio posits that semaglutide and chemically similar drugs, also known as analogues, may influence addictive behaviors because they affect not just the gut but the brain as well. He believes semaglutide and other GLP-1 analogues might inhibit the release of dopamine, a neurotransmitter that evokes the feeling of pleasure after smoking and drinking. Regardless, although people claim Ozempic is repressing their nail-biting and online shopping habits, pharmaceutical companies are not actively studying the effects of GLP-1 drugs on addiction. It is clear that more thorough research is required before confirming any causal links.
Pharmaceutical companies are, however, already developing more potent relatives of semaglutide which mimic more than just GLP-1. Tirzepatide, sold under brand names like Mounjaro, mimics both GLP-1 and the gut hormone GIP. The drug was approved in 2022 for treating Type 2 diabetes and for weight loss just last November. If this was not enough, a third drug known as retatrutide, which stimulates GLP-1, GIP and glucagon — another hormone involved in hunger regulation — is in the works and helped people lose up to an astounding 24% of their body weight after 48 weeks of treatment. These drugs are diversifying in their function and in what other health benefits they provide, increasing the number of patients they can treat.
That being said, Ozempic and similar drugs carry a few thorns with their roses. Semaglutide can cause stomach aches, constipation, diarrhea, nausea, vomiting and other unsavory side effects. Rapid, significant weight loss can cause gallbladder disease, which is also an occasional complication of bariatric surgery. Worryingly, semaglutide and GLP-1 analogues have been shown to melt away muscle mass along with body fat, posing a significant concern for older users. What’s more, patients using these drugs for weight loss likely will not experience lasting results if they stop taking their medication. Thus, semaglutide and its relatives do not necessarily provide a sustainable method of keeping any lost weight off.
Needless to say, Ozempic usage has exploded in Hollywood and mainstream media for its weight-loss effects. Celebrities such as Oprah Winfrey, Elon Musk and Amy Schumer have admitted to trying these medications to lose stubborn body fat; although Ozempic is officially for Type 2 diabetes, it can be prescribed with the off-label use of aiding in weight loss. Unfortunately, the usage of semaglutide has reached a point where many Americans in actual need of these medications cannot fill their prescriptions. From 2020–22, prescriptions for these drugs increased by 300%, almost reaching nine million prescriptions by the end of 2022. The FDA included both Ozempic and Wegovy on its drug shortages list in 2023. Furthermore, with the drugs’ high cost — Wegovy costs nearly $1,350 per month without insurance — and with variable insurance coverage, many people with Type 2 diabetes or a life-threatening level of obesity cannot access the medication they need.
Semaglutide drugs have spawned all sorts of media coverage and Internet jokes like calling stick-skinny Christmas trees “Ozempic trees.” However, their prevalence necessitates a longer conversation about other unexpected benefits, class disparity and healthcare access in the United States. We must continue researching how we can use GLP-1 analogues to our advantage and make them accessible to those in need, not just the rich and famous looking to lop off their love handles.